Table of Contents
Toggle
Toxicological emergencies can strike anyone, anywhere. An आपातकालीन देखभाल सहायक (ECA) or Emergency Medical Technician (EMT) plays a vital role in the initial response and management of these critical situations. While definitive treatment falls to medical doctors, an ECA’s or EMT’s swift and informed actions can make a world of difference. In this blog, we will explore toxicological emergencies and also discuss approaches to deal with it.
Understanding Toxicological Emergency
A toxicological emergency arises when an individual is exposed to a harmful substance (toxin) in sufficient quantity to cause adverse health effects or Cardio-Pulmonary compromise. These toxins can be ingested, inhaled, absorbed through the skin, or injected.
Common Causes of Poisoning
- Opioids
- Organophosphates
- Salicylates
- Carbon dioxide Poisoning
- Overdose of Prescribed Medicines
- Cocaine and Stimulant Drugs of Abuse
- Antidepressants
- Barbiturates
Various Routes of Toxic Exposure
Inhalation
This is the most common route of exposure. Inhalation may occur in the form of vapours, gases, mist, or dust particles. e.g- Carbon monoxide gas, chlorine gas, or ammonia vapours, environmental pollutants, industrial chemicals gases, etc.
Ingestion
Entry of toxic substances into the body through the mouth, usually by swallowing. e.g- accidental ingestion of household chemicals like cleaning products, pesticides, overdose or misuse of medicines prescribed or over the counter, ingestion of poisonous plants or mushrooms, etc.
Dermal Contact or Absorption
Exposure or contact of the skin to toxins, like acids or alkalis, irritants, allergens, corrosive chemicals, toxic plants, splashes or spills, or contact with contaminated objects, etc.
Injection
Toxic substances can enter the body through injection through skin and muscles, like contaminated needle or syringes, animal bites or stings or the injection of illicit drugs, synthetic opioids, anaesthesia or pain killer drug misuse.
Toxidromes
Toxidromes are a set of clinical signs and symptoms associated with specific classes of toxins or drugs. Recognition of a toxidrome can help diagnose the cause of poisoning and direct treatment. ECAs and EMTs need to consider the patient’s clinical presentation, history of exposure, and physical examination findings when identifying a toxidrome and determining the appropriate management approach. Prompt recognition and intervention can help prevent complications and improve outcomes for patients affected by toxic exposures.
The particular symptoms of a toxidrome will depend on the toxin involved, but some common symptoms include:
- Altered mental status (confusion, drowsiness, coma)
- Nausea and vomiting
- Diarrhea
- Seizures
- Abnormal vital signs (heart rate, respiratory rate, blood pressure)
- Dilated or constricted pupils
- Dry, flushed skin
- Diaphoresis (excessive sweating)
- Urinary incontinence
- Urinary retention
Management of Toxicological Emergencies
Role ECAs/EMTs during three crucial stages:
1. Primary Assessment
The priority during transport is the ABCDE approach, ensuring critical life functions are addressed:
- A – Airway:
- Ensure an open airway by tilting the head back and lifting the chin.
- Remove any visible obstructions from the mouth or throat.
- If necessary, insert an oral airway or use a suction device.
- B – Breathing:
- Assess the patient’s breathing rate, depth, and effort.
- Administer oxygen if breathing is compromised.
- Be prepared to assist ventilation with a bag-valve-mask or ventilator if needed.
- C – Circulation:
- Check for a pulse and assess its rate, strength, and regularity.
- Control any external bleeding with direct pressure and dressings.
- If indicated, establish intravenous (IV) access and administer fluids.
- D – Disability:
- Perform a quick neurological assessment to determine the level of consciousness using tools like the AVPU (Alert, Verbal, Pain, Unresponsive) scale.
- Assess pupillary responses and potential seizure activity.
- E – Exposure:
- Look for environmental clues (e.g., empty containers, spills, and unusual odours) that might indicate the cause of the patient’s condition.
- This information can be vital in identifying potential toxins and guiding further treatment.
2. Triage Management
Upon arrival, a rapid assessment helps determine the severity of the poisoning and guide further management:
- History: past, present, event, medical history. Talk to the patient or family to understand the potential exposure.
- Physical Examination: Vital signs, skin changes, pupils, and potential seizure activity.
- Triage Score: To prioritise the patient’s management.
- Look for specific signs and symptoms of the suspected toxin (e.g., pinpoint pupils for opioids, miosis for organophosphates).
Neurological Assessment in Triage: Glasgow Coma Scale (GCS)
GCS is a neurological assessment tool designed to evaluate a patient’s level of consciousness as a way to assess the severity of a brain injury.
The GCS assesses three key aspects of responsiveness:
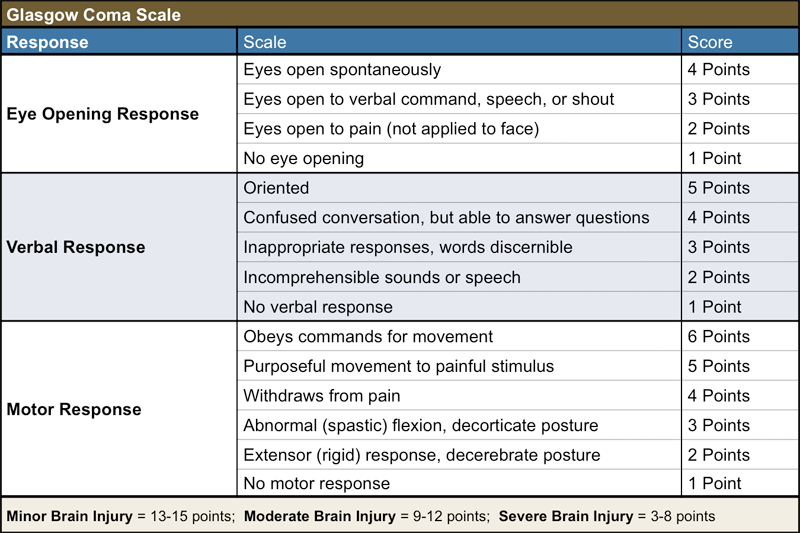
Interpretation of GCS Scores:
- A score of 13–15 generally indicates no brain injury or non-significant brain injury.
- 9–12: moderate brain injury.
- 8 or below- severe brain injury that requires immediate medical attention.
ECAs and ETAs can use the GCS score alongside other assessments to determine the best course of treatment.
Arterial Blood Gases Test (ABG)
An ABG test is a crucial diagnostic tool that measures the levels of various gases and the acid-base balance in a patient’s blood.
By measuring parameters such as pH, PaO2, PaCO2, bicarbonate (HCO3-), and oxygen saturation (SaO2), ABG helps in:
- Assessing Acid-Base Balance: Respiratory acidosis or alkalosis, metabolic acidosis or alkalosis, or mixed disorders. This information is vital for diagnosing underlying conditions and guiding appropriate interventions.
- Evaluating Oxygenation Status: PaO2 indicates the adequacy of oxygen exchange in the lungs, while SaO2 indicates the oxygen-carrying capacity of hemoglobin.
- Monitoring Respiratory Function: PaCO2 reflects the effectiveness of pulmonary ventilation and helps in diagnosing respiratory disorders such as hypoventilation or hyperventilation.
Key ABG parameters:
- pH: normal (7.35-7.45, acidosis (pH < 7.35), or alkalosis (pH > 7.45).
- PaCO2: Normal: 4.5–6 OkPa. Elevated levels of respiratory acidosis, decreased levels of respiratory alkalosis.
- HCO3-: Normal: 22–26 mmol/L. Elevated levels of metabolic alkalosis and decreased levels of metabolic acidosis.
- PaO2: Normal: 10.7–13.3 kPa. Decreased levels-hypoxemia.
- SaO2: Normal: > 95%; decreased levels of hypoxemia.
ECAs and EMTs can effectively use this tool to ultimately improve patient outcomes and save lives.
3. Further Management
- Antidote Administration: If a specific antidote is available and indicated, administer it by following the established protocols.
- Gastric Decontamination: In some cases, gastric lavage (pumping the stomach) or administration of activated charcoal might be employed to remove unabsorbed toxins. However, these procedures require careful consideration.
- Seizure Management: If seizures occur, medications might be administered to control them.
- Decontamination Procedures: If the poison is on the skin or eyes, continue irrigation with copious amounts of water.
- Temperature Control: If the patient is hypothermic (has an abnormally low body temperature), implement measures to prevent heat loss and raise body temperature. This may involve using blankets or warming packs. Conversely, if the patient is hyperthermic (abnormally high body temperature), initiate cooling measures like removing excess clothing, applying cool compresses, or using other cooling techniques.
- Monitoring and Supportive Care: Continuously monitor vital signs, administer oxygen as needed, maintain temperature control, and provide supportive care (pain management, fluids).
निष्कर्ष
Toxicological emergencies present complex challenges that require a multidisciplinary approach and effective collaboration among ECAs, EMTs, and doctors. By understanding the above information, ECAs, and EMTs can better prepare themselves to respond to these critical situations and mitigate their impact on patients and communities. Tech Mahindra SMART Academies for Healthcare are focused on providing a thorough understanding of poisoning and its management to ECAs and EMTs. We provide practical skills with the help of expert trainers.

