Table of Contents
ToggleThe incidence of pressure injuries has traditionally been viewed as an indicator of quality nursing care. The provision of basic nursing care is one of the primary functions of a nurse. The recent advances and challenges in healthcare have ushered in a new era where the role of a majority of healthcare professionals has evolved and transformed to meet the demands of an ever-changing care continuum. The role of the allied health professionals has undergone a transition with increased responsibilities and functionalities. One such role is that of the nursing assistant.

Role of a Nursing Care Assistants
The nursing assistants are often called the ‘eyes and ears ‘of the nurse. As a nursing assistant, you will perform activities ranging from:
- Giving bed baths
- Assisting with perineal care
- Positioning and repositioning of patients
- Feeding patients
- Providing back care
- Changing linen, and
- Observing and reporting any changes in the patients’ condition
You are the initial and the final point of contact for patients, one of the main reasons in the contribution you can make towards improving care outcomes and participating in the provision of quality healthcare to a patient.
What is a Pressure Injury?
Ulcers are common in 9% of the people in hospitals, 3 to 12% in nursing homes and 3 to 14% of people being cared for at home. People transferred from hospitals to nursing homes are particularly vulnerable, with 10 to 35% having sores when they are admitted to the nursing home.
The word ‘Pressure Injuries’ often raises a patient safety alarm for many involved in the care of that patient. The incidences of Hospital-acquired Pressure Injuries (HAPI) not only causes significant harm to the patient by delayed recovery but also results in substantial quality and cost issues to the hospital. Prevention is, therefore, the best bet in the management of a pressure injury. Nursing Care Assistants must be familiar with the basics of pressure injury and prevention strategies.
A pressure injury is the localized damage to the skin and underlying soft tissue usually over a bony prominence or related to medical or other devices. (NPUAP, 2016)
Unrelieved pressure on the skin squeezes tiny blood vessels, which supply the skin with much-needed nutrients and oxygen. When the skin is starved for too long, the tissue dies and a pressure ulcer forms.
How does a Pressure Injury occur?
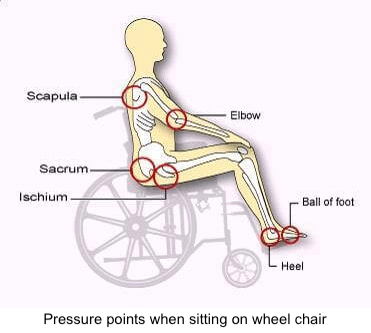
The most common causes of a pressure injury are friction, shear, moisture, impaired physical mobility, prolonged pressure over a bony prominence causing a reduction in the blood flow to a particular area and resultant skin damage. The most common locations for a pressure injury are the back of the head, shoulder blade, elbow, heel, lower back, hip, ear, and heel.
Ulcers form where the weight of the person’s body presses the skin against the firm surface of a bed or chair. In people confined to bed, ulcers are most common over the following parts of the body:
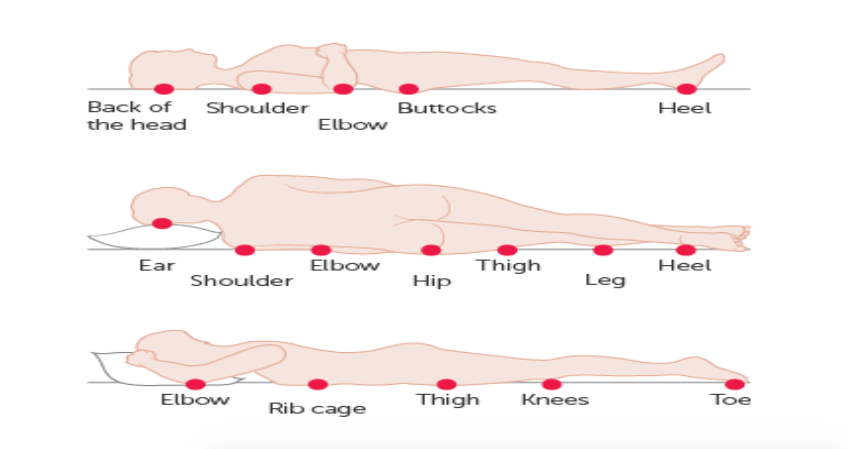
Pressure points during Supine, Lateral and Prone position
This pressure from prolonged lying or sitting temporarily cuts off the skin’s blood supply. This injures skin cells and can cause them to die. Unless the pressure is relieved and blood flows to the skin again, the skin soon begins to show signs of injury.
 At first, there may only be a patch of redness. If this red patch is not protected from additional pressure, the redness can form blisters or open sores. In severe cases, damage may extend through the skin and create a deep crater that exposes muscle or bone. Muscle is even more prone to severe injury from pressure than skin. A mild injury to the skin may cover a deeper, more pronounced injury to the muscle.
At first, there may only be a patch of redness. If this red patch is not protected from additional pressure, the redness can form blisters or open sores. In severe cases, damage may extend through the skin and create a deep crater that exposes muscle or bone. Muscle is even more prone to severe injury from pressure than skin. A mild injury to the skin may cover a deeper, more pronounced injury to the muscle.
The pressure that causes ulcers does not have to be very intense. Applying pressure which is less than 25% of the pressure of a normal mattress can also lead to ulcers. Normally, our skin is protected from being injured by this pressure because we move frequently, even when we sleep.
Although pressure on the skin is the main cause of ulcers, other factors often contribute to the problem. Some most of the most common factors that can cause pressure injury:
- Decreased Movement: Ulcers are common in people who can’t move because of various reasons such as severe arthritis, obesity, stroke and multiple sclerosis. People who can move with little or no assistance have a lower risk of ulcers because they can shift their weight occasionally.
- Decreased Sensation: Ulcers are common in people who have neurological problems that decrease the ability to feel or verbally express pain or discomfort. Without these feelings, the person cannot feel the effects of prolonged pressure on the skin.
- Circulatory Problems: People with atherosclerosis, circulatory problems from long term diabetes or localized swelling (Edema) may be more likely to develop ulcers. This is because the blood flow in their skin is weak even before the pressure is applied to the skin. People with anemia are also at risk because their blood cannot carry enough oxygen to skin cells, even though circulation may be normal.
- Poor Nutrition: Studies show that ulcers are more likely to develop in people who don’t get enough protein, vitamins C & E, calcium or zinc.
- Shearing & Friction: Shearing and friction causes the skin to stretch and blood vessels to kink, which can impair blood circulation in the skin. If a person is confined to bed, shearing & friction can occur when the person is dragged or slid across the bedsheets. This can also occur when the head of the bed is raised more than 30 degrees. This increases shearing forces over the lower back & tailbone.
- Moisture: Wetness from perspiration, urine or faeces can make the skin too soft & more likely to be injured by pressure. For this reason, people who can’t control their bladders or bowels (incontinent) are at high risk of developing ulcers.
- Age: Elderly people, especially those over 85, are more likely to develop ulcers because skin usually becomes thinner with age. Also, as we age, the fat tends to shift away from the body surface, where it acts as a cushion, to deeper areas of the body.
How do we grade a pressure injury?
A pressure injury is graded into four stages:
- Stage 1: Intact skin with non-blanchable redness
- Stage 2: Partial-thickness skin loss involving epidermis, dermis or both.
- Stage 3: Full-thickness tissue loss with fat.
- Stage 4: Full-thickness tissue loss with exposed bone, muscle or tendon.
Ulcers can lead to severe medical complications, including bone & blood infections, infectious arthritis, and holes below the wound that burrow into bone or deeper tissues, and scar carcinoma, a form of cancer that develops in scar tissue.
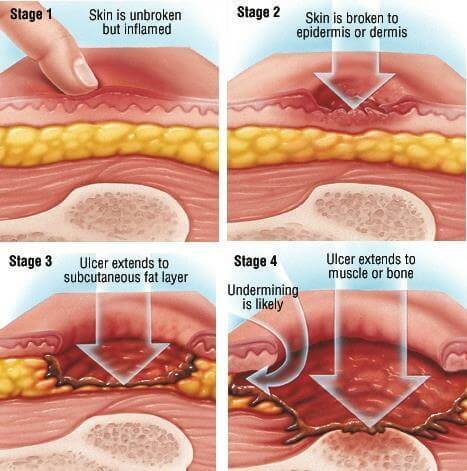 Stages of Pressure Injury
Stages of Pressure Injury
- Stage 1st: Early sign of skin damage in people with pale skin develops a lasting patch of red skin that does not turn white when you press it with your finger. In darker skin, the patch may be more difficult to detect.
- Stage 2nd: The injured skin blister or develops an open sore or abrasion that does not extend through the full thickness of the skin. There may be a surrounding area of red or purple discolouration, mild swelling and some oozing.
- Stage 3rd: The ulcer becomes the crater that goes below the skin surface.
- Stage 4th: The crater deepens and reaches into a muscle, bone, tendon or joint.
Because broken skin is a prime spot for bacteria, ulcers are extremely vulnerable to infection. This is especially true if the sore is contaminated by urine or faeces. Signs of infection in an ulcer can include:
- Pus draining from the sore
- A foul-smelling odour
- Tenderness, heat and increased redness in the surrounding skin
Prevention of Pressure Injuries
Healthcare experts believe that at least 50% of ulcers can be prevented by using simple measures to relieve pressure and decrease the skin’s vulnerability to injury. To help prevent ulcers in a person who is confined to a bed or chair, the healthcare professional should create and follow a plan of care individualized to each person. The plan may include these strategies:
1. Relieve pressure on vulnerable areas: Change the person’s position every two hours when in bed and every hour when sitting in a chair. Use pillows to raise the person’s arms, legs buttocks & hips. Relieve pressure on the back with an egg-crate foam mattress or a water mattress.
Use pillows or foam wedges to keep boney prominences such as knees and ankles from direct contact with each other. Teach chair bound people, who are able, to shift their weight every 15 minutes. Do not use donut devices!
2. Reduce Shear & Friction
- Avoid dragging the person across the bedsheets. Either lift the person by using a lift sheet or have the person use an overhead trapeze to briefly raise their body.
- Keep the bed free from crumbs and other particles that can rub and irritate the skin.
- Do not raise the head of the bed more than 30 degrees, unless they are eating in bed or the doctor tells you otherwise.
- Use boots & elbow pads to reduce friction on heels and elbows. Elevate heels on pillows if boots are not used.
- Wash the person gently. Avoid rubbing or scrubbing the skin and make sure they are thoroughly dry.
- Inspect the person’s skin at least once each day. Early detection can prevent a Stage I redness from becoming worse.
3. Minimize irritation from chemicals: Avoid irritating antiseptics, hydrogen peroxide, povidone-iodine solution (Betadine) or other harsh chemicals to clean or disinfect the skin.
4. Encourage the person to eat well: The diet should include enough calories, protein, calcium, zinc and vitamin C & E. If the person cannot eat enough food, offer nutritional supplements. Ask the doctor about ordering vitamin supplements.
5. Encourage daily exercise: Exercise increases blood flow and speeds healing. In many cases, even bedridden people can do stretches and simple exercises.
6. Keep the skin clean and dry: Clean the skin with a non-irritating, non-drying soap. Avoid hot water. Dry skin well. Use absorbent pads to draw moisture away from vulnerable areas. If the person is incontinent try to find ways to control or limit the number of incontinent episodes. Toilet the person regularly. Check for wetness several times a day and provide incontinent care. Do not let a person sit or lay in bed wet for long periods. Use topical moisture barriers. Lotion skin well to prevent dryness and cracking. Do not massage over bony prominences.

5-step model to prevent pressure ulcer
Prognosis
In many cases, the outlook for ulcers is good. Prevention and early detection is the ultimate situation that can be accomplished with care and understanding by all. Remember, you are a part of the healthcare team and can play a significant role in communicating and contributing to the provision of holistic care to a patient. Prevention always remains with us: Comfort, Contact points, Continence, Circulation, Communication, Complete care.


